Victoria’s healthcare system at breaking point
HEALTHCARE and the healthcare system are at the top of most people’s minds. If it’s not the out-of-pocket gap when seeing a GP, then it’s trying to get in to see a specialist. One specialist clinic on the Peninsula (the closest to Bass Coast)...

HEALTHCARE and the healthcare system are at the top of most people’s minds.
If it’s not the out-of-pocket gap when seeing a GP, then it’s trying to get in to see a specialist.
One specialist clinic on the Peninsula (the closest to Bass Coast) has a wait until February and that is for private patients, patients then face triaging with those deemed less urgent facing a greater wait.
Those across Gippsland are feeling the brunt, in Wonthaggi alone, both GP clinics are now mixed billing predominantly due to inadequate Medicare rebates.
The Royal Australian College of General Practitioners (RACGP) has warned that general practice care needs a much-needed shot in the arm, a statement echo by Dr Rob Phair who believes a bigger conversation must be had.
A recent HealthEd survey of almost 500 GPs found 22 per cent had recently changed their billing model, up 12 per cent on last year.
One-third of those who changed their billing model moved from bulk billing to mixed billing, and 67 per cent changed from mixed billing to completely private billing.
Rising practice costs and Medicare cuts were listed as key reasons for the billing changes.
A local clinic
Locally the sentiments are echoed.
“We’ve always been mixed billings,” Wonthaggi Medical Group Practice Manager, Gayle Bloch explained.
“I think doctors that previously were prepared to bulk bill are starting to pull back.
“Costs of running practices, with the pandemic, are continuing to increase. You don’t want to make it all about money, but our dollar has to stretch a lot further; the only way to recoup that is to pass it on to the patient.”
Wonthaggi Medical Group like many other practices had to put on additional staff during the pandemic, and with COVID still heavily impacting the industry staff shortages are being felt and with it the increased costs.
“We expect people to hand sanitise and wear a mask, if they don’t have one, they’re provided.
“That costs a considerable amount of money. Things are starting to settle a little bit and we’re finding supplies are coming back to pre-pandemic costs, but for a while, the markup was astronomical.”
No truer example of supply and demand, clinics felt the full force of increased costs as supply shortages were faced the world over; masks over triple their previous cost.
“Things that didn’t cost you much to provide suddenly did.”
As masks are no longer required in public, clinics like Wonthaggi are facing a new dilemma – patients not having a mask on them.
“People turn up without them, because they don’t have them in their bags and in their pockets, they don’t have to put them on every time they go out. You’re having to start to hand things out more regularly again.”
With Medicare rebates increasing by 1.6 per cent, equating to 65 cents for a standard consult, Gayle admits an adequate increase would assist.
“It still wouldn’t alleviate the need for private fees, but it would help,” Gayle explained.
“The government goes out and says the CPI is going up five per cent. But how do you pay that five per cent to every staff member here? We haven’t had a five per cent increase in our revenue.
“We don’t charge patients for dressings, they come out of that bottom line as well.
“The amount we spend on dressings is astronomical, but you want to make sure people have got quality products.
“If you drop your quality you end up using more product anyway and causing more follow up for a patient, it’s not something we want to have to do.
“We’re trying to save patients being in their pocket.”
For Gayle, the concern is people not getting the health care they need, and the pressure on doctors from patients to continue bulk billing.
Another balancing act on the scales is attracting and keeping good doctors.
“To be able to afford to still give quality care and to attract doctors to the practice, again, it’s not about money, but people need to know they can earn an income, a reasonable income to come to a job, like anyone else.
“Attracting quality doctors, being able to use quality products and equipment to provide quality care, you don’t want to lower the care you provide but somehow you have to be able to pay for it.
“But in doing that, you don’t want people to not get the health care they need because I feel, with everything else, everyone’s getting hit everywhere.”
Clinics are also advising patients to be open and have a conversation.
“We’ve had people say I can’t afford to get that procedure done; I haven’t got the money.
“Talk to us, there is always a way to make sure we can help you get the care you need.
“And please be kind.”
For the patient
Juxtaposing the clinics are those receiving the care.
Earlier this year we reported on women’s health, and the demand for an increase of $3.70 per woman. A meagre increase would save on average $13,647 per woman in the future (or $41.2billion).
How does someone who cannot afford to put sufficient fresh produce on their table, afford $22.10 each time they genuinely need to see a doctor?
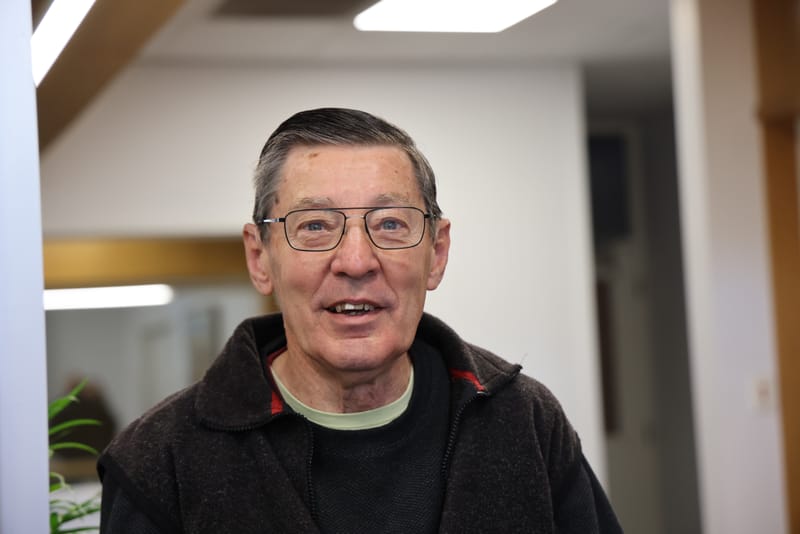
Well-known Wonthaggi resident Jessica Harrison has seen the effects firsthand in her many voluntary roles with low-income households.
“It will seriously affect disadvantaged people who can’t afford private health insurance – that’s the first thing,” Jessica stated.
“And it may mean that people just don’t take the opportunity to have surgery, which may prevent them from more extreme illness or immediate living with pain.
“It’s a very worrying development.



“I hope that the situation will be resolved quickly so that people on low incomes are not disadvantaged by this.”
As Jessica explains, “there is a problem with funding these operations, that needs to be resolved so that hospitals and doctors can do their work without the unfair disadvantage to people who are on fixed incomes and low incomes.”
“In my work as a career I’ve come across many situations where people are waiting on operations. It’s already a stressful situation to be waiting with health concerns, but then whether you will be able to afford that gap, that’s just another added stress.
“It seems the costings haven’t really kept up with the time.
“When I first came to Wonthaggi 20 years ago there was no bulk billing at the doctors. That situation was sorted out and so it would be terrible if that started to happen to people who need surgery, and other medical interventions.”
A regional medical stance
As the Sentinel-Times delved into the topic, we spoke with Dr Rob Phair, President of the Rural Doctors Association of Victoria, who is also based in East Gippsland.
“There’s a really dramatic shortage of GP’s,” Dr Phair said.
“That’s the first issue and then you have to look at the underlying issues and the background; the reasons are pretty complex; they’ve got a significant drop off from junior doctors and medical students interested in training. Part of it is because it’s not as prestigious, part cultural, medicines become much more sub specialised, everyone wants to be a super sub specialist. Then you pick medical students that come from Melbourne, they’ll want to stay in Melbourne. There are all kinds of factors.
“And then bulk billing. The problem with bulk billing is really significant.
“GP practices are run as a small business, their costs are going up significantly and the rates you get back for consultations with Medicare are basically going backwards, it’s completely unsustainable.
“A lot of Gippsland is pretty low income, and to get the care (low-income households) need they will ideally not be paying for it. Basically, someone has to pay, you have to finance the care somehow.
“Tristar is a famous example, there are none in Gippsland, but they basically went into receivership, and they had clinics all around country Victoria. You get doctors from overseas, try to get patients in as quickly as possible and then bulk bill everyone.”
Increasing the Medicare rebate may help solve part of the problem but is not the answer according to Dr Phair.
“We need to have a bigger, broader conversation, the problem is bigger than just the Medicare rebate.
“If you look at the commentary by people like Steven Duckett from the Grattan Institute and other critiques, we need to work out how we’re funding health services; it’s really confusing. The federal
Department of Health fund Medicare, and yet you’ve got state governments running hospitals, and what we’re finding in Gippsland, is that a lot of people can’t get into GPs, or they don’t want to pay for it, therefore, they show up at the emergency department.
“They get the care at no cost but wait for a long time, and they don’t get the continuity of care; there are all kinds of flow on effects.”
Dr Phair also highlighted the problem with the bulk billing model.
“You basically get paid for getting people in the door and that favours certain types of medicines.
“For example, the stereotype is the older GP who is able to get someone in and out the door in five minutes, deals with one issue, they’ll bulk bill them and then move on to the next patient, whereas female GPs who do a lot of mental health care are really disadvantaged by that.
“We have to think about how what kind of care we want to provide and how we fund it, and that’s a really big conversation.”
Dr Phair also addressed the political issues tied to health care and policies, which are particularly targeted and driven by where governments need votes but agreed that the Modified Monash criteria was a good policy.
The Modified Monash Model: is a measure of remoteness, looks at incentives and support in specific areas; for our community, Phillip Island, Wonthaggi, Inverloch and Leongatha fall under MM4 – medium rural town, surrounding areas in between and across to Yarram and Port Welshpool are deemed MM5 – small rural towns, and French Island and Sunday Island are MM6 – remote communities.
“Be organised when you go to your GP – make a priority list. Make sure you spend that time well and address what’s really worrying you the most,” Dr Phair said.
“I don’t really want to suggest it but if you’re originally from Melbourne you might consider continuing to get medical care back in Melbourne because it’s much less under the pump.
“We have to think about what we value; people spend huge amounts of money on smartphones, and yet their upset about paying to see their GP, sometimes people undervalue their health.
“I’m not saying people should be paying for health care, but I think it’s worth taking the time to think about how you spend your money and what matters to you.”
Dr Phair also recommends using other sources – ask your pharmacist about your medications, practice nurses where a GP may not be necessary and a physio for musculoskeletal concerns.
And write to your parliamentarians.
“Say we’re desperately short of GP’s – they do pay attention.”
The Medicare Levy and Politics
Minister for Health and Aged Care, Mark Butler was recently on Triple J – Hack, and explained the problem from the top.
“What we have seen over the last 10 years are cuts and neglect to Medicare – unsurprisingly doctors have had to reduce their level of bulk billing or where they do charge gap fees to see those fees climb higher and higher,” Mr Butler said.
“For the first time in the 40-year history of Medicare the average gap fee that people are paying for a standard consult with their GP is more than the Medicare rebate itself – that has never been the case before.
“It’s never been harder to get into a doctor than it is right now, and it’s never been so expensive.
“We’ve got a taskforce that is meeting on a monthly basis between now and Christmas to work out how best to spend ($250million that is committed to Medicare) – whether that is an increase to the rebate, employing more nurses… Next year the money will start to flow.”
And lastly, but not least the question on everyone’s mind – ‘I’m paying a Medicare Levy, where is it going?’
According to the latest tax statistics from the ATO, for the 2019-2020 tax period 10,417,278 individuals (of 14,958,590) paid the Medicare levy with a total figure of $17.2 billion.
Of those individuals, a further 411,624 paid the Medicare levy surcharge equalling $502 million.
Health expenses that are funded through the Medicare and private health insurance rebate include delivering essential health services, including public hospitals, the Pharmaceutical Benefits Scheme (PBS), Repatriation Pharmaceutical Benefits Scheme, Aboriginal and Torres Strait Islander health programs, mental health services and health workforce initiatives.
The DisabilityCare Australia Fund is funded from the 0.5 per cent to 2 per cent increase in the Medicare levy in recent years.
According to the federal Budget 2020-21, the actual expenses figure for Health 2019-20 was $87.023 billion.
Jumping to the Budget 2021-22, the Health Portfolio – Department of Health had an estimated actual opening balance of $1.628billion and other Health Portfolio accounts totalling $412million.